Most American families encounter myths about bipolar disorder that are far from the truth. More than 4 percent of American adults will experience serious mood swings associated with bipolar disorder at some point, making it a widespread concern. Understanding the real symptoms and common misconceptions can empower you to recognize early warning signs, seek the right support, and challenge the stereotypes that often stand in the way of meaningful recovery.
Table of Contents
- Defining Bipolar Disorder and Common Myths
- Types of Bipolar Disorder and Key Differences
- Core Symptoms: Mood Swings and Behavioral Signs
- How Bipolar Disorder Affects Addiction Recovery
- When and How to Seek Professional Help
Key Takeaways
| Point | Details |
|---|---|
| Understanding Bipolar Disorder | Bipolar disorder is a serious neurobiological condition involving significant mood fluctuations that need professional treatment. |
| Types of Bipolar Disorder | There are three main types: Bipolar I, Bipolar II, and Cyclothymic Disorder, each requiring tailored treatment approaches. |
| Mood Episodes and Symptoms | Mood swings during manic and depressive episodes drastically affect daily functioning, necessitating a careful assessment for effective management. |
| Seeking Professional Help | Early recognition of symptoms and seeking mental health intervention can lead to improved outcomes and emotional stability. |
Defining Bipolar Disorder and Common Myths
Bipolar disorder is a complex mental health condition characterized by significant mood fluctuations that extend far beyond typical emotional experiences. This neurological condition involves dramatic shifts between periods of intense emotional highs (mania) and devastating lows (depression), disrupting an individual’s ability to function consistently in daily life.
Contrary to popular misconceptions, bipolar disorder is a serious medical condition that requires professional treatment. Myths surrounding this disorder persist and can prevent individuals from seeking necessary help. Some pervasive myths include the belief that bipolar disorder is simply mood swings or a character weakness, when in reality, it is a complex neurobiological condition involving neurotransmitter imbalances and genetic predispositions.
The primary types of bipolar disorder include Bipolar I, characterized by more severe manic episodes, and Bipolar II, which involves less intense hypomanic periods. Key diagnostic characteristics involve understanding the duration, intensity, and frequency of mood episodes. People experiencing bipolar disorder often cycle through various emotional states, which can significantly impact their relationships, professional performance, and overall quality of life. Understanding these nuanced distinctions helps mental health professionals provide more targeted and effective treatment strategies.
Recognizing bipolar disorder’s complexity requires dispelling harmful stereotypes and promoting compassionate, evidence-based understanding. Treatment typically involves a comprehensive approach including medication, psychotherapy, lifestyle modifications, and ongoing support. Individuals struggling with this condition should feel encouraged to seek professional help, as modern treatment approaches can effectively manage symptoms and support long-term emotional stability.
Types of Bipolar Disorder and Key Differences
Bipolar disorder encompasses several distinct diagnostic categories, each characterized by unique patterns of mood episodes and severity. The National Institute of Mental Health identifies three primary classifications of bipolar disorder, each representing a different spectrum of emotional experiences and challenges.
Bipolar I Disorder represents the most intense form of the condition, marked by dramatic manic episodes lasting at least seven days that often require hospitalization. These manic periods can involve extreme behavioral changes, including grandiose thinking, reduced need for sleep, and potential psychotic symptoms. In contrast, Bipolar II Disorder demonstrates less severe mood fluctuations, characterized by hypomanic episodes that are shorter and less disruptive, alongside more pronounced depressive periods.
The third classification, Cyclothymic Disorder, represents a milder version of bipolar disorder. Individuals experience numerous periods of hypomanic and depressive symptoms that do not meet the full diagnostic criteria for major episodes. These mood shifts are more frequent but less intense, creating a persistent emotional instability that can significantly impact daily functioning. Each type requires a nuanced understanding and personalized treatment approach that considers the specific symptom patterns and individual needs.
Understanding these distinctions is crucial for accurate diagnosis and effective treatment. Mental health professionals carefully assess the duration, frequency, and intensity of mood episodes to determine the appropriate bipolar disorder subtype. While each type presents unique challenges, comprehensive treatment strategies involving medication, psychotherapy, and lifestyle modifications can help individuals manage symptoms and achieve emotional balance.
Core Symptoms: Mood Swings and Behavioral Signs
Mood swings represent the hallmark characteristic of bipolar disorder, creating a complex emotional landscape that dramatically impacts an individual’s daily functioning. The National Institute of Mental Health identifies these mood episodes as the core diagnostic criteria for understanding the disorder’s progression, with each phase presenting distinct behavioral and psychological symptoms.
During manic episodes, individuals typically experience an intense surge of energy, creativity, and impulsivity. These periods are characterized by rapid speech, decreased need for sleep, grandiose thinking, and potentially risky behaviors such as excessive spending, sexual impulsivity, or engaging in dangerous recreational activities. Comprehensive research from the Substance Abuse and Mental Health Services Administration highlights how these symptoms can significantly disrupt personal and professional relationships.
Conversely, depressive episodes represent the opposite emotional extreme, marked by profound sadness, extreme fatigue, feelings of hopelessness, and potential suicidal ideation. Individuals may experience significant changes in sleep patterns, appetite, and cognitive functioning, often struggling with concentration, decision making, and maintaining basic daily responsibilities. These depressive periods can be particularly dangerous, as the stark contrast with manic episodes can create a sense of emotional exhaustion and psychological vulnerability.
Understanding these symptomatic variations is crucial for effective management and treatment. Mental health professionals carefully assess the duration, intensity, and frequency of these mood episodes to develop personalized intervention strategies. While the experience of bipolar disorder is deeply individual, recognizing these core symptoms can help individuals seek appropriate support, engage in comprehensive treatment, and develop effective coping mechanisms to navigate the complex emotional landscape of this challenging condition.
How Bipolar Disorder Affects Addiction Recovery
Substance use disorders frequently co-occur with bipolar disorder, creating a complex psychological landscape that significantly challenges traditional recovery approaches. Extensive research into the intricate relationship between mental health and addiction reveals profound interconnections that complicate treatment strategies, highlighting the need for comprehensive, integrated intervention methods.
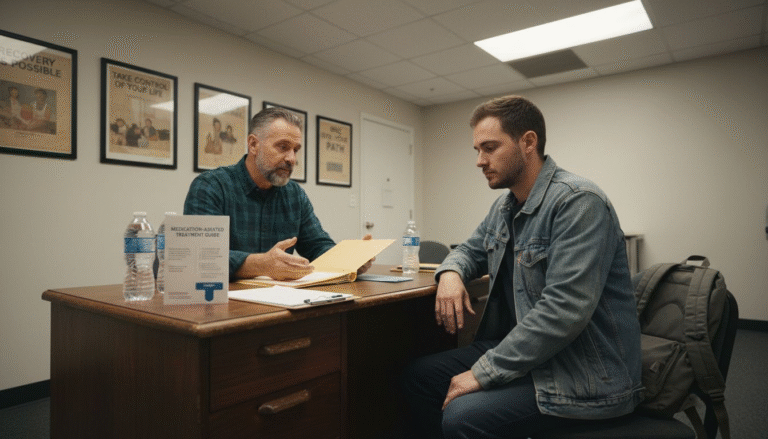
Individuals with bipolar disorder often turn to substances as a form of self-medication, attempting to manage overwhelming emotional fluctuations. Manic episodes can trigger impulsive drug or alcohol use, while depressive periods might drive individuals to seek temporary relief through substance consumption. This cyclical pattern creates a dangerous feedback loop where addiction and bipolar symptoms continuously exacerbate each other, making comprehensive treatment approaches that address both conditions simultaneously crucial for successful recovery.
The recovery process for individuals with co-occurring bipolar disorder and addiction demands a nuanced, multidisciplinary approach. Mental health professionals must carefully balance medication management for bipolar symptoms while simultaneously addressing substance dependency. Integrated treatment strategies typically involve specialized psychotherapy, mood stabilization, relapse prevention techniques, and ongoing support systems that recognize the unique challenges presented by dual diagnoses.
Successful recovery requires recognizing that bipolar disorder and addiction are not isolated conditions, but deeply interconnected experiences that demand holistic, compassionate intervention. Bipolar Disorder and Addiction: Complete Guide provides individuals and their support networks with essential insights into navigating these complex psychological challenges. By understanding the intricate relationship between mood disorders and substance use, patients can develop more effective coping mechanisms and create sustainable paths toward long-term healing and emotional stability.
When and How to Seek Professional Help
Mental health intervention represents a critical step in managing bipolar disorder, requiring individuals to recognize subtle yet significant warning signs that indicate professional support is necessary. The National Institute of Mental Health provides comprehensive guidelines for identifying when specialized psychiatric assistance becomes essential, emphasizing the importance of early recognition and proactive treatment.
Critical warning signs that demand immediate professional consultation include persistent mood instability, prolonged periods of depression or mania lasting more than two weeks, significant disruptions in work or personal relationships, and experiencing recurring suicidal thoughts. Mental health professionals recommend seeking support when symptoms interfere with daily functioning or create potential safety risks, highlighting the importance of understanding one’s emotional and psychological boundaries.
The initial consultation with a mental health professional typically involves a comprehensive psychological assessment, including detailed medical history, symptom tracking, and potential diagnostic evaluations. Mental health programs can help individuals navigate complex psychological challenges by providing personalized treatment strategies that address individual needs. Treatment approaches may include a combination of psychiatric medication, psychotherapy, lifestyle modifications, and ongoing support systems designed to stabilize mood and improve overall quality of life.
Ultimately, seeking professional help is an act of courage and self-preservation. Recognizing that bipolar disorder is a treatable medical condition—not a personal weakness—can empower individuals to take critical steps toward recovery. Mental health professionals offer compassionate, evidence-based interventions that can transform challenging emotional experiences into opportunities for growth, stability, and meaningful personal development.
Take Control of Bipolar Disorder and Addiction Recovery Today
Living with bipolar disorder means facing intense mood swings that can disrupt your daily life and complicate addiction recovery. The article highlights how symptoms like manic impulsivity and depressive lows can create a dangerous cycle with substance abuse. If you or a loved one are struggling with these challenges, feeling overwhelmed, or uncertain about how to navigate co-occurring disorders, you are not alone. Addressing the complex emotional and behavioral signs of bipolar disorder alongside addiction requires specialized, compassionate care.
At Glendora Recovery Center, we understand the critical importance of integrated treatment tailored to your unique experience. Our comprehensive programs combine medication management, psychotherapy, and flexible scheduling options including Partial Hospitalization Programs and telehealth sessions to fit your life. Don’t wait until symptoms control your future. Reach out now to our experienced team for personalized support and take the first step toward stability. Contact us today via our website and begin your path to recovery with trusted professionals who care.
Frequently Asked Questions
What are the common symptoms of bipolar disorder?
Common symptoms include intense mood swings between mania and depression, with manic episodes involving increased energy, grandiose thinking, and impulsivity, while depressive episodes feature sadness, fatigue, and possible suicidal thoughts.
How does bipolar disorder affect addiction recovery?
Bipolar disorder often co-occurs with substance use disorders, as individuals may self-medicate during manic or depressive episodes. This interconnected relationship can complicate treatment, necessitating integrated approaches to address both conditions simultaneously.
When should I seek professional help for bipolar disorder?
Seek professional help if you experience persistent mood instability, prolonged depressive or manic periods lasting more than two weeks, significant disruptions in daily life, or recurring suicidal thoughts.
What treatment options are available for managing bipolar disorder?
Treatment typically involves a combination of medication, psychotherapy, lifestyle modifications, and ongoing support tailored to individual needs, aimed at stabilizing mood and enhancing overall quality of life.