Juggling work or family in Los Angeles County while fighting addiction can make traditional treatment options feel out of reach. Intensive Outpatient Programs offer a structured path to recovery with 9 to 19 hours per week of therapy, education, and counseling so you never have to choose between help and your responsibilities. Discover how an Intensive Outpatient Program gives you intensive support for substance abuse and co-occurring mental health challenges while you keep your life on track.
Table of Contents
- Defining Intensive Outpatient Programs For Addiction
- Key Features And Structure Of IOP Care
- Types Of Intensive Outpatient Programs Available
- Eligibility, Admission, And Core Requirements
- Costs, Insurance, And Legal Considerations
- Comparing IOP To Other Treatment Options
Key Takeaways
| Point | Details |
|---|---|
| Intensive Outpatient Programs (IOPs) provide flexibility. | IOPs allow individuals to maintain daily responsibilities while receiving 9 to 19 hours of treatment weekly. |
| Dual diagnosis is a key focus. | IOPs address both substance abuse and co-occurring mental health conditions, crucial for effective recovery. |
| Variety of program types are available. | Options include standard, evening/weekend, telehealth, dual diagnosis, and family-integrated IOPs to meet different needs. |
| Commitment is essential for success. | Regular attendance at scheduled sessions is crucial for effective treatment and maintaining progress. |
Defining Intensive Outpatient Programs for Addiction
An Intensive Outpatient Program (IOP) is a structured treatment approach designed for people struggling with substance abuse who don’t require full-time hospitalization or medical detoxification. Unlike residential programs where you stay overnight, IOPs let you maintain your daily responsibilities while receiving professional care.
IOPs typically provide 9 to 19 hours per week of treatment sessions. This time commitment includes group therapy, individual counseling, family therapy, and educational classes focused on addiction recovery and mental health. The structure is intensive without being all-consuming, which makes it realistic for people in Los Angeles County who are working, managing family obligations, or handling other life responsibilities.
What sets IOPs apart is flexibility. You attend scheduled sessions during mornings, evenings, or weekends depending on your situation. If you’re dealing with both substance abuse and a co-occurring mental health condition like depression or anxiety, the program addresses both simultaneously. This dual diagnosis approach is crucial because untreated mental health issues often drive relapse.
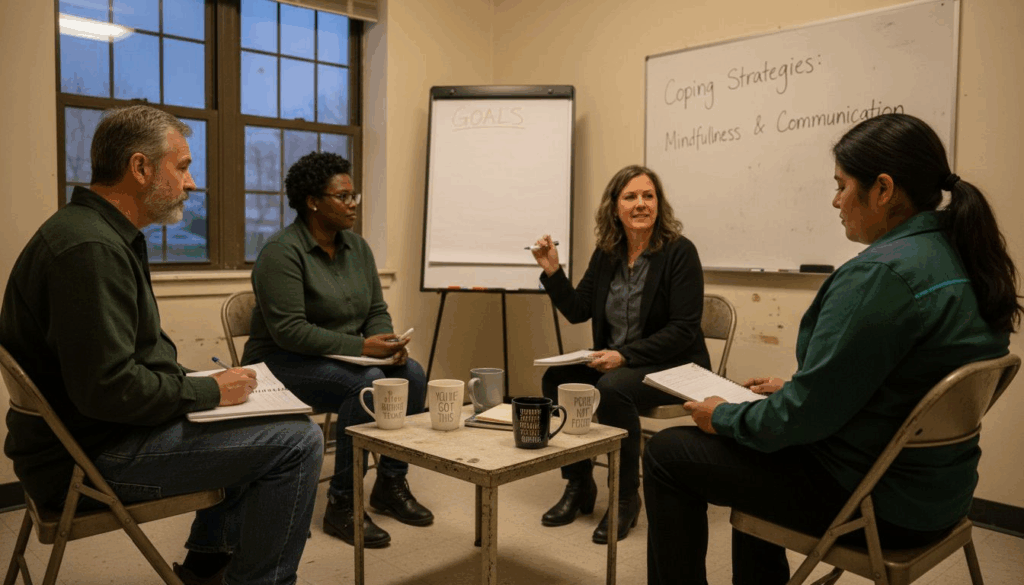
The core components include structured therapy sessions where you work with licensed counselors on triggers and coping strategies. Group therapy connects you with others facing similar battles, reducing the isolation that often fuels addiction. Family therapy helps repair relationships damaged by substance use and builds a support system at home.
IOPs exist in the middle ground between outpatient counseling and inpatient hospitalization. You get clinical oversight and evidence-based treatment without losing your independence or daily routine. This model works particularly well for adults who have stabilized enough to live safely at home but need more support than weekly therapy appointments provide.
Understanding how intensive outpatient programs work helps you evaluate whether this level of care matches your recovery needs.
Pro tip: When selecting an IOP, confirm it offers flexible scheduling that actually fits your work hours and family commitments, and ask specifically about co-occurring mental health treatment options.
Key Features and Structure of IOP Care
IOPs operate on a clearly defined framework that balances clinical intensity with practical flexibility. The structure is built around regular, consistent attendance rather than living at a facility. You show up for scheduled sessions, receive treatment, and return home to your life, your job, your family.
The backbone of IOP treatment is 9 to 19 hours per week of structured programming. This isn’t sitting passively in lectures. You’re actively engaged in counseling sessions, educational classes, and therapeutic work designed specifically for addiction and mental health recovery. The mix includes both individual therapy where you work one-on-one with a counselor and group sessions where you connect with peers in recovery.
Group therapy serves as the foundation of most programs. Being in a room with others who understand addiction firsthand cuts through the shame and isolation that often keeps people stuck. You hear stories similar to yours, challenge unhelpful thinking patterns together, and build accountability with people who genuinely get what you’re facing.
Individual sessions with a therapist dig deeper into your personal triggers, history, and recovery goals. These are tailored to your specific situation, whether you’re managing anxiety, depression, trauma, or all three alongside substance abuse. Mental health professionals create customized treatment plans that address your exact needs rather than a one-size-fits-all approach.
Scheduling flexibility is intentional. Morning sessions, evening appointments, and weekend options exist because recovery happens in the real world where people work and care for families. You’re not choosing between your job and your recovery. The program adapts to fit your life constraints.
Most programs run from several weeks to several months. The timeline depends on your progress and needs. You’re not locked in indefinitely, but you’re not expected to fix years of addiction in weeks either.
Pro tip: Ask your IOP about their specific therapy modalities (cognitive behavioral therapy, motivational interviewing, family therapy) and confirm they offer evening sessions that don’t conflict with your work schedule.
Types of Intensive Outpatient Programs Available
IOPs aren’t one-size-fits-all. Different programs serve different needs, and understanding the variations helps you find the right fit for your specific situation. Los Angeles County offers several types of intensive outpatient treatment, each designed with particular populations or challenges in mind.
Standard IOPs focus on substance abuse recovery with integrated mental health support. These programs serve adults dealing with alcohol or drug addiction alongside conditions like anxiety, depression, or trauma. The emphasis is on dual diagnosis treatment, recognizing that untreated mental health issues sabotage recovery. You’ll work with counselors trained in both addiction and psychiatry.
Evening and weekend IOPs cater specifically to working professionals and parents. If your job doesn’t allow midday appointments or your family responsibilities are rigid, these programs adjust. Sessions run after work hours or on Saturdays, making treatment compatible with your existing commitments. This flexibility doesn’t mean less intensive care, just differently timed care.
Telehealth IOPs have expanded access significantly. You attend sessions online from home, eliminating commute time while maintaining full treatment intensity. This works well for people managing transportation barriers or preferring privacy. The clinical quality remains identical to in-person sessions.
Dual diagnosis or psychiatric IOPs serve people with serious mental health conditions alongside substance use. If you’re managing bipolar disorder, schizophrenia, severe depression, or complex trauma while struggling with addiction, these specialized programs have staff trained in managing both simultaneously. The psychiatrist and therapists coordinate closely.
Family-integrated IOPs involve your support system directly. Rather than treating you in isolation, these programs include family sessions, education, and therapy specifically designed to repair relationships and build household accountability. If your family dynamic contributes to relapse risk, family involvement becomes treatment itself.
Here’s a quick reference of common types of Intensive Outpatient Programs and who benefits the most from each:
| IOP Type | Ideal Participant | Unique Advantage |
|---|---|---|
| Standard | Adults with addiction | Dual diagnosis support |
| Evening/Weekend | Working professionals, parents | Scheduling flexibility |
| Telehealth | Remote/local residents | No commuting required |
| Dual Diagnosis | Severe mental health cases | Close psychiatric coordination |
| Family-Integrated | Families with strained ties | Healing and accountability |
Learning more about IOP benefits and treatment approaches helps you determine which type aligns with your recovery needs and life circumstances.
Pro tip: When comparing programs, ask whether they offer the specific schedule that works for you and whether their staff specializes in your particular combination of substance use and mental health conditions.
Eligibility, Admission, and Core Requirements
Not everyone enters an IOP at the same point in their recovery journey. Eligibility depends on your current stability, medical needs, and readiness for outpatient-level care. Understanding these criteria helps you know whether an IOP is appropriate for you right now.
The primary requirement is that you don’t need medical detoxification or 24-hour hospital monitoring. If you’re actively withdrawing from alcohol or benzodiazepines, you need inpatient medical care first. IOPs assume you’ve either already completed detox or don’t require it. Your body needs to be medically stable enough to attend sessions without constant supervision.
You must be willing and able to commit to regular attendance. This isn’t optional. Missing sessions undermines your treatment and peers’ recovery. Programs typically require you to show up for scheduled appointments consistently, whether that’s mornings, evenings, or weekends. If you can’t commit to the time requirement, an IOP won’t work.
Basic stability matters. You need safe housing where you can return after each session. Homelessness or unsafe living situations complicate outpatient treatment because you lack a stable base to practice recovery skills. Many programs coordinate with supportive housing services if this is a barrier.
Mental health readiness is crucial. Assessment for co-occurring mental health conditions helps clinicians determine if you need psychiatric medication management alongside therapy. If you’re experiencing active psychosis, severe suicidality, or untreated bipolar disorder, the program may refer you to more intensive care initially.
Most programs require an initial assessment, sometimes called an intake evaluation. During this appointment, clinical staff ask detailed questions about your substance use history, mental health, medical status, medications, and life circumstances. This assessment determines your treatment plan and identifies any urgent safety concerns.
Age requirements vary. Some IOPs serve adults only, typically starting at age 18. Others have adolescent programs with different structures and staffing. Verify the program’s age eligibility before applying.
Pro tip: During your intake assessment, be completely honest about your mental health symptoms, medication use, and any suicidal thoughts or safety concerns, as this directly affects treatment planning and your safety in the program.
Costs, Insurance, and Legal Considerations
IOP treatment involves real financial costs, but several pathways can make care affordable. Understanding insurance coverage, out-of-pocket expenses, and financial assistance options prevents cost from becoming a barrier to recovery.
Insurance coverage for IOPs has expanded significantly. Medicare began covering intensive outpatient services as of January 2024, improving access for older adults. Most private insurance plans also cover IOPs, though coverage varies. Your specific plan determines what percentage of costs you pay and whether you meet a deductible first.
The actual cost of treatment depends on location, program length, and services included. IOP costs vary widely based on these factors, and insurance coverage details like copayments and deductibles differ among providers. A program in Los Angeles County might cost differently than one in rural areas. Always ask about total costs upfront before enrolling.
If you lack insurance, don’t assume treatment is impossible. Many IOPs offer sliding scale fees based on income. Some programs provide financial assistance or payment plans. Government-funded treatment programs exist for uninsured or underinsured residents. Call ahead to ask about affordability options.
Privacy rights matter legally. Treatment records are protected under HIPAA, meaning your information stays confidential. Employers cannot access your treatment details. The only exceptions involve court orders, imminent danger, or specific legal circumstances. Understand these protections upfront.
State licensing regulations ensure clinical quality. Programs must meet staffing standards, maintain proper credentials for clinicians, and follow evidence-based practices. This isn’t arbitrary bureaucracy, it’s your assurance that trained professionals deliver care. Verify a program’s licensing before enrolling.
Pro tip: Call your insurance company before selecting an IOP and ask specifically about coverage percentages, deductible status, and whether prior authorization is required, then confirm that information directly with the program.
Comparing IOP to Other Treatment Options
Addiction treatment exists on a spectrum. Where you land depends on your medical stability, severity of use, work obligations, and support system. IOPs occupy the middle ground, offering more structure than standard therapy but more freedom than residential programs.
Standard outpatient therapy typically involves one therapy session per week for 50 minutes. You’re working with a counselor or therapist, but the time commitment is minimal and the structure is loose. This works for people with mild addiction or strong self-motivation. If you’re struggling with severe substance abuse or complex trauma, weekly sessions won’t interrupt destructive patterns enough.
Inpatient or residential programs require you to live at the facility full time. You’re there 24 hours a day, seven days a week, sometimes for 28 days or longer. Medical staff monitor you constantly. This level suits people who need structured supervision, medical management, or who’ve repeatedly failed outpatient treatment. The trade-off is losing independence and time away from work and family.
Partial hospitalization programs sit between IOPs and inpatient care, offering more hours than IOPs but less than full hospitalization. You attend 5 or more hours daily but return home at night. This works if you need intensive structure but have evening family responsibilities or a stable home environment.
IOPs fit people who need more support than weekly therapy but can maintain a job or family role. You’re attending 9 to 19 hours weekly, getting real treatment intensity without losing your independence. This model suits Los Angeles County adults juggling work and recovery.
The following table compares the structure and benefits of major addiction treatment levels:
| Approach | Weekly Time Commitment | Patient Independence | Clinical Intensity |
|---|---|---|---|
| Outpatient Therapy | 1 hour per week | Full home/work life | Low |
| Intensive Outpatient | 9-19 hours per week | Home/work life maintained | Moderate (group, individual, family) |
| Partial Hospitalization | 25+ hours per week | Evenings at home | High |
| Residential/Inpatient | 24 hours/day | Facility-based, no outside work | Very high (medical and constant care) |
The choice isn’t permanent. You might start residential treatment, step down to an IOP, then transition to outpatient therapy. Or you might realize standard outpatient isn’t enough and upgrade to an IOP. Treatment flexibility allows adjustment based on your actual progress and needs.
Understanding how different treatment levels work together helps you recognize when to escalate or de-escalate care intensity.
Pro tip: Discuss your work schedule and family responsibilities directly with the admissions counselor so they can recommend the treatment level that realistically fits your life instead of what looks good on paper.
Find the Right Intensive Outpatient Program for Your Lasting Recovery
Struggling to balance addiction recovery with everyday responsibilities can feel overwhelming. This article highlights the challenges people face when seeking a flexible, yet structured Intensive Outpatient Program that addresses both substance abuse and mental health conditions. If you need an IOP that fits your work hours, supports co-occurring disorders, and offers both in-person and telehealth options, Glendora Recovery Center has the solution.
Our upscale treatment facility in Glendora, CA, specializes in comprehensive programs tailored to your unique needs. We provide Intensive Outpatient Programs with flexible scheduling including mornings, evenings, weekends, and online sessions. Our team focuses on dual diagnosis care and family therapy to help rebuild relationships while promoting accountability.
Take the next step toward recovery today by reaching out to discuss how our Intensive Outpatient Programs can fit your life without sacrificing treatment quality. Learn more about our holistic approach on our Contact Page and connect with caring professionals ready to support your journey. Don’t wait to get the personalized help you deserve—visit Glendora Recovery Center now and begin transforming your life.
Frequently Asked Questions
What is an Intensive Outpatient Program (IOP) for addiction?
An Intensive Outpatient Program (IOP) is a structured treatment option for individuals struggling with substance abuse that does not require full-time hospitalization. It allows participants to maintain their daily responsibilities while receiving professional care, typically involving 9 to 19 hours of treatment weekly.
How do I know if I am eligible for an Intensive Outpatient Program?
Eligibility for an IOP typically requires that you do not need medical detoxification or 24-hour monitoring. You must be willing to commit to regular attendance and have a safe living situation. An initial assessment is usually conducted to determine if the program is appropriate for you.
What types of therapy are included in an Intensive Outpatient Program?
IOPs generally offer a mix of group therapy, individual counseling, family therapy, and educational classes. These therapies address both addiction and any co-occurring mental health conditions, aiding in a comprehensive recovery approach.
What makes an IOP different from other treatment options?
IOPs provide more structure and intensive programming than standard outpatient therapy, while offering more independence than inpatient or residential treatment. This makes IOPs suitable for those who need substantial support but can still manage work and family commitments.
Recommended
- Everything You Need to Know About Intensive Outpatient
- IOP | Intensive Outpatient Program | Glendora Recovery Center
- Intensive Outpatient Program: Who This Is For?
- Intensive Outpatient Program Teens Can Get Effective Results
- Amazon Reinstatement Services for Rapid Seller Account Recovery | Reddog Consulting Group
- Ikigai FAQ: Complete Guide to Finding Your Purpose | Ikigain